Functional dyspepsia, also known as non-acid dyspepsia, is characterized by discomfort and pain involving the upper gastrointestinal tract. It is a common condition that is present in 15–20 percent of the population. Symptoms are often mistaken for acid reflux disease, but functional dyspepsia is a separate entity, though there can be overlap.
Similarly, patients with functional dyspepsia can also have symptoms of irritable bowel syndrome, so the diagnosis can often be missed. However, correct identification of this condition can help guide treatment.
Clinical Presentation
Functional dyspepsia is categorized into epigastric pain and postprandial distress syndrome. Epigastric pain syndrome is bothersome epigastric pain and/or burning that occurs at least once a week, while postprandial distress syndrome is typically related to meals. It applies to bothersome postprandial fullness and/or early satiation that occurs at least three days a week and is severe enough to impact regular activities or prevent the finishing a regular-size meal.
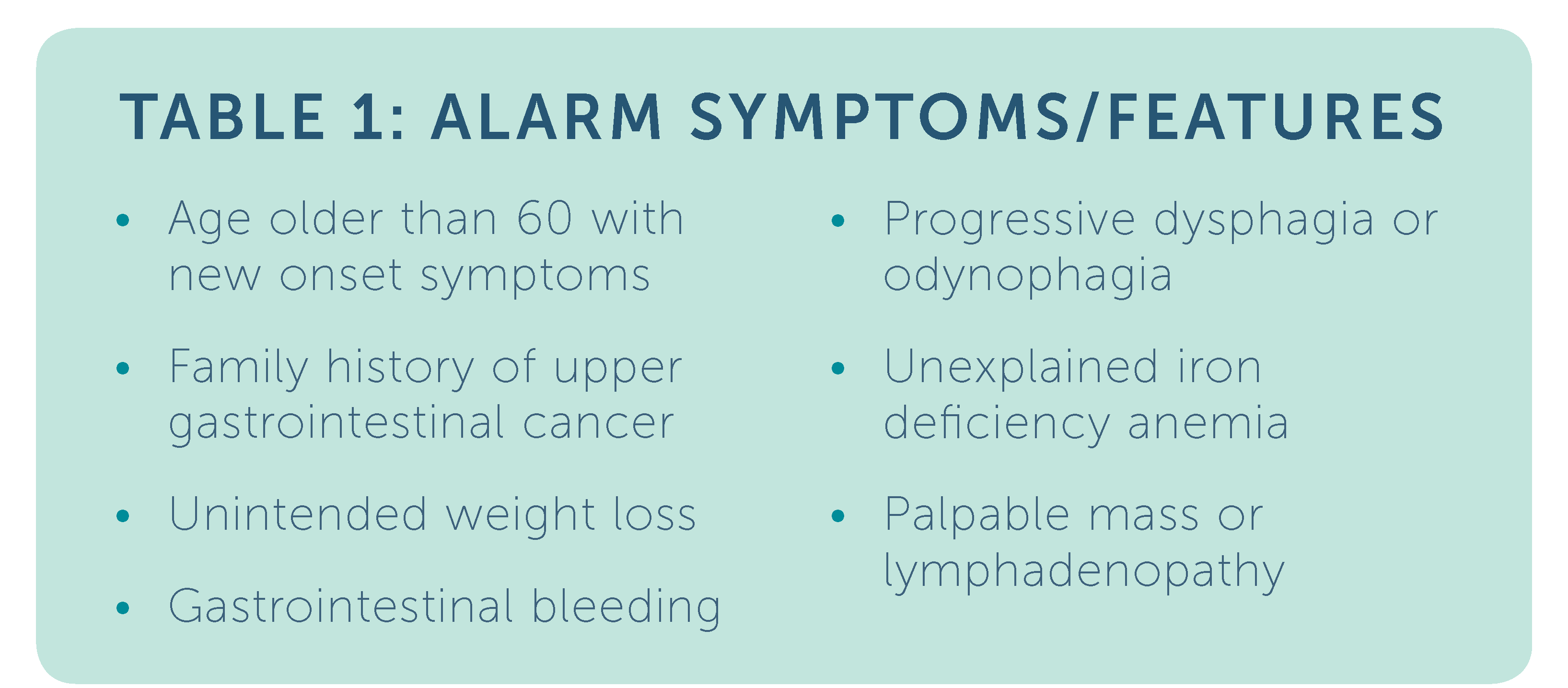
Symptoms should have occurred in the past three months and have a duration of at least six months. A key criteria is the absence of structural disease. Excessive belching and nausea can also be present, however vomiting should prompt workup for an alternative diagnosis. The alarm features listed in Table 1 should prompt endoscopic evaluation.
Pathophysiology
The pathogenesis of functional dyspepsia is still under research. Studies suggest that visceral hypersensitivity leads to the symptom of pain. Mildly elevated duodenal eosinophils have also been identified in those with functional dyspepsia. This finding suggests that a low-grade inflammatory state, potentially from food antigens or previous infections, may be a contributing factor. More research is needed to determine the significance of this finding and its treatment implications.
Other studies have shown that a subset of patients with H. pylori have symptom resolution after eradication, particularly in those with epigastric pain as a symptom, so testing and treatment for this has been incorporated into guidelines. Impaired gastric accommodation after meals has been noted in functional dyspepsia as well. Under normal physiologic conditions, the fundus of the stomach should relax to accommodate the ingestion of a meal, but this function can be impaired in those with postprandial distress, leading to symptoms of early satiety in the absence of delayed emptying.
Treatment
Current recommendations for those without alarm symptoms (see Table 1) include testing and treatment for H. pylori. Symptom resolution can take up to six to twelve months, so patients should be advised that symptoms may not resolve immediately. If H. pylori eradication is not effective, treatment can then be guided based on the functional dyspepsia subtype. Acid suppression therapy with proton pump inhibitors or H2 receptor antagonist therapy have been shown to be superior to placebo. They are effective for both subtypes of functional dyspepsia.
In those with predominantly postprandial distress symptoms, prokinetics or medications that relax the fundus (buspirone or mirtazapine) can help alleviate symptoms. Tricyclic antidepressants can be helpful in those with predominantly epigastric pain. Reassurance that there is no associated increased mortality as well as treatment of underlying stress are important adjuncts to pharmacologic therapy.