
Colorectal cancer (CRC) is the third most common cancer in the US, and the incidence is increasing in younger people. The USPSTF now recommends starting CRC screening at age 45 instead of 50.1
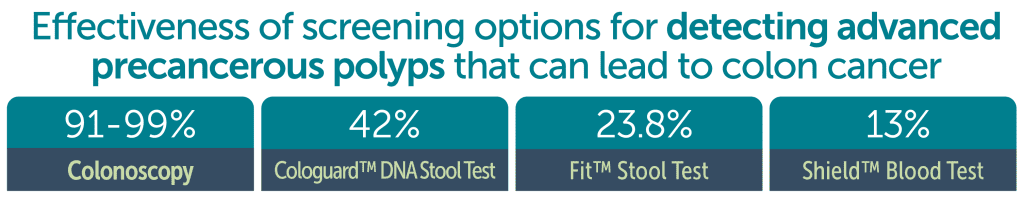
Although multiple tests are approved for CRC screening, colonoscopy, which is both diagnostic (100% detection rate for colon cancer)2 and therapeutic (allows the ability to remove precursor or “precancerous” polyps), remains the gold standard for CRC screening. The procedure is overall very safe (4-8 complications in 10,000 patients) and if no polyps or cancer are found, could potentially be done every ten years. Read our related story about insurance coverage for colonoscopy.
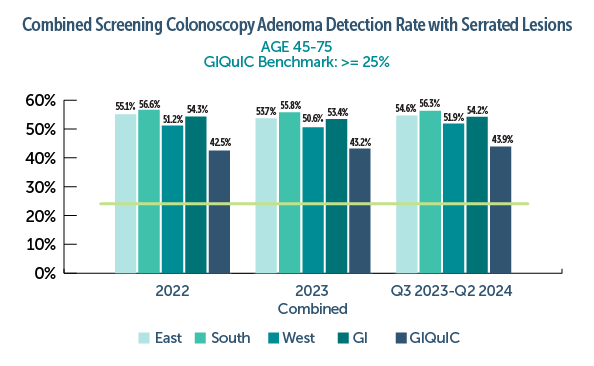
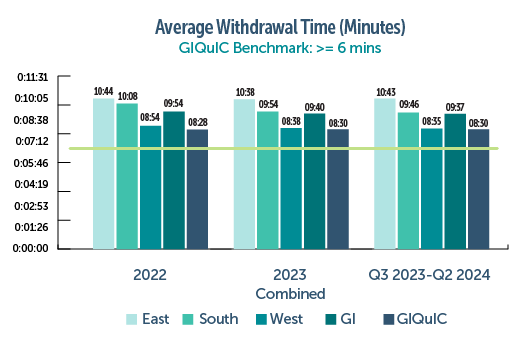
In general, high-quality colonoscopies are defined by meeting certain quality metrics that lead to better patient outcomes, including reduced incidence and mortality related to CRC. Colonoscopy quality indicators were recently updated in September 2024.3 Two of the most widely reported and evidence-based quality metrics include adenoma detection rate (ADR) and average withdrawal time. ADR was increased (> 35% for male and females) and now includes patients 45 or older with expanded indications beyond screening. A sessile serrated lesion (SSL) detection rate was also added; previously these types of polyps were included in the traditional ADR. Finally, increasing average withdrawal time was recommended, as longer withdrawal times have been shown to increase ADR.
Furthermore, when considering where to refer a patient for their procedure, a colonoscopy performed by a gastroenterologist is generally considered the preferred option compared to a surgeon. Gastroenterologists perform a significantly higher volume of colonoscopies, and procedures done by a gastroenterologist are associated with reduced risk from developing colon cancer,4 and a higher likelihood of meeting quality benchmarks.5
The Oregon Clinic GI East, South, and West locations (TOC GI) collect quality data for every outpatient colonoscopy performed and historically outperforms the national average for essentially every metric, even compared to the new recommended benchmarks. For example, combined data from all TOC GI locations in 2024 shows:
- ADR for both traditional adenomas and sessile serrated lesions for males and females ages 45 to 75 was 55% on screening colonoscopy (national average 44%, updated benchmark > 35% for traditional adenomas and > 6% recommended for SSLs).
- Average withdrawal time on a screening colonoscopy was 9 minutes 35 seconds (national average was 8 minutes 30 seconds, updated benchmark > 8 minutes).
TOC GI also performs very well against benchmarks set for common colonoscopy complications. In 2024:
- Post-polypectomy bleeds in 0.06% procedures (benchmark <1%)
- Perforations in 0.01% procedures (benchmark <0.2%)
- Aspiration in 0.03% procedures (benchmark <0.1%)
Thus, the case is made to recommend a screening colonoscopy for your patient at TOC GI, where quality metrics are exceeded and complication rates are very low. Please reach out to us for screening colonoscopy referrals—our wait lists have significantly reduced, and we are able to see patients much sooner than in the past.
References
1. US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–1977.
2. Shaukat et. al. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. The American Journal of Gastroenterology 116(3):p 458-479, March 2021.
3.Rex et. al. Quality Indicators for Colonoscopy. The American Journal of Gastroenterology 119(9):p 1754-1780, September 2024.
4. Baxter et. al. Association Between Colonoscopy and Colorectal Cancer Mortality in a US Cohort According to Site of Cancer and Colonoscopist Specialty, J Clin Oncol. 2012 Jun 11;30(21):2664–2669.
5. Muthukuru et. al. Quality of Colonoscopy: A Comparison Between Gastroenterologists and Nongastroenterologists, Comparative Study Dis Colon Rectum. 2020 Jul;63(7):980-987.



