Endoscopic Retrograde CholangioPancreatography (ERCP)
ERCP is short for Endoscopic Retrograde CholangioPancreatography.
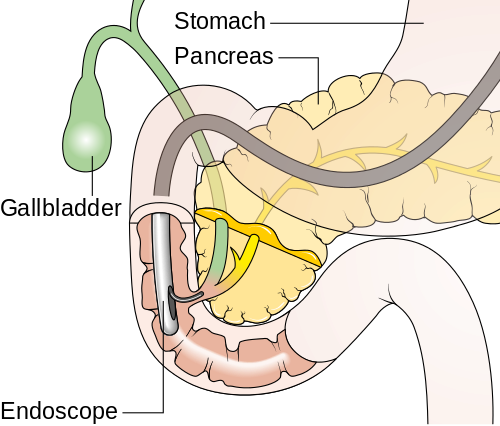
Endoscopic refers to the use of an instrument called an endoscope – a thin, flexible tube with a tiny video camera and light on the end. The endoscope is used by a highly trained subspecialist, the gastroenterologist, to diagnose and treat various problems of the GI tract. The GI tract includes the stomach, intestine, and other parts of the body that are connected to the intestine, such as the liver, pancreas, and gallbladder.
Retrograde refers to the direction in which the endoscope is used to inject a liquid enabling X-rays to be taken of the parts of the GI tract called the bile duct system and pancreas. The process of taking these X-rays is known as cholangiopancreatography. Cholangio refers to the bile duct system, pancrea to the pancreas.
What to Expect
What You Can Expect During an ERCP
X-ray equipment is then used to examine and take pictures of the dye outlining the ducts. In this way, widening, narrowing, or blockage of the ducts can be pinpointed.
Some of the problems that may be identified during ERCP can also be treated through the endoscope. For example, if a stone is blocking the pancreatic or common bile duct, it is usually possible to remove it.
First, the opening in the papilla is cut open and enlarged. Then, a special device can be inserted to retrieve the stone. Narrowing or obstruction can also have other causes, such as scarring or tumors. In some cases, a plastic or metal tube (called a stent), can be inserted to provide an opening. If necessary, a tissue sample or biopsy can be obtained, or a narrow area dilated.
What Will Happen
- The nurse and doctor will talk to you about the test and answer any questions you have. You should know why you are having an ERCP and understand the treatment options and possible risks. You will be asked to sign a consent form, which gives the doctor your permission to do the test, and any necessary treatment.
- You will put on a hospital gown. You will be asked to remove any eye glasses, contact lenses or dentures. An IV will be started and blood may be drawn for lab studies. You may receive antibiotics through the IV at this time.
- You will be taken by stretcher to the procedure room. The nurse will help you get into the correct position, usually on your side, and make you comfortable. A clip on your finger and cuff on your arm will help the nurse monitor your pulse, blood pressure and oxygen level.
Everything Will be Done to Ensure Your Comfort
- ERCP is done under sedation or anesthesia, depending on the complexity of the case, your past experiences with endoscopy procedures, and mindful of your wishes. Sedation makes you relaxed and sleepy. Anesthesia means deep sedation supervised by an anesthesiologist, or full anesthesia with a temporary breathing tube.
- A suppository may be placed in the anus at the start of the procedure to reduce the risk of pancreatitis.
- You will be given medicine through the IV to make you relaxed and sleepy.
- A medicine will be sprayed onto the back of your throat to make it numb. The medicine may taste unpleasant but it will stop any coughing during the test.
- A plastic guard will be placed between your teeth to protect them.
- When you are sleepy, the doctor will place a thin, flexible tube (endoscope) through the mouth guard and into your mouth.
- The doctor will then ask you to swallow. When you swallow, the endoscope will gently move down your esophagus, the same way food goes down when you are eating. You may feel like gagging, but you should not feel any pain. The endoscope will not interfere with your breathing. If sedation is used:
- After you are sedated or anesthetized, the doctor will guide the endoscope through your esophagus, stomach and duodenum. The doctor will use it to inspect the lining of your stomach and duodenum. You should not feel any pain, but you may have a sense of fullness, since air may be introduced to help advance the scope.
- In the duodenum, the instrument is positioned near a small opening of the bile and pancreatic ducts called the papilla of Vater. The papilla is the point at which the main bile and pancreatic ducts empty into the intestine.
- The doctor will then place a small plastic tube (catheter) through the endoscope into the papilla. It can be directed into either the pancreatic or common bile duct. Guidewires and contrast material (dye) will be placed into the ducts, and x-ray pictures are taken.
- The doctor may take samples and can provide treatment for many problems. Details are given below.
- ERCP usually lasts between 30 and 90 minutes.
- You may be given indomethacin, a medicated suppository, while you are asleep to help prevent pancreatitis.
Watch and learn about the ERCP procedure to remove a stone in the bile duct.
Warning: Contains graphic video
Treatments During ERCP
If the x-ray pictures taken during ERCP show a stone or blockage in the ducts, the doctor may be able to treat the problem right away. Common treatments are sphincterotomy, stone removal and stenting.
- Sphincterotomy. This involves making a small cut in the Ampulla of Vater (using an electric knife) to enlarge the opening to the bile duct and/or pancreatic duct. This is done to improve the drainage or to remove stones in the ducts. Removed stones are usually dropped in the intestine, and pass through quickly.
- Stone removal. Small stones may be removed by small balloons, baskets or other devices.
- Stenting. A stent is a tube which is placed in a blocked or narrowed duct to improve drainage. The narrowing may need to be stretched (dilated) before the stent is placed. A few stents are designed to pass out into the intestine after a few weeks when they have done their work. Other stents have to be removed or changed after 3-4 months. There are also permanent stents made out of metal mesh.
Other treatments are used occasionally. Your doctor will explain these if necessary.
What You Can Expect After Your ERCP
You will be taken on a stretcher to the recovery area to relax. Your blood pressure and heart rate are watched while you rest. You will be fully awake in about 30 minutes. If treatments were done during your test, you may need to be observed in hospital overnight.
When your ERCP is completed on an outpatient basis, you will need to remain under observation until your doctor or healthcare team has decided you can return home. Sometimes, admission to the hospital is necessary.
When you do go home, be sure you have arranged for someone to drive you, since you’re likely to be sleepy from the sedative you received. This means, too, that you should avoid operating machinery for a day, and not drink any alcohol.
Your doctor will tell you when you can take fluids and meals. Usually, it is within a few hours after the procedure. Because of the air used during ERCP, you may continue to feel full and pass gas for awhile, and it is not unusual to have soft stool or other brief changes in bowel habits. However, if you notice bleeding from your rectum or black, tarry stools, call your doctor.
You should also report vomiting, severe abdominal pain, weakness or dizziness, and fever over 100 degrees. Fortunately, these problems are not common.
ERCP is an effective and useful procedure for evaluating or treating a number of different problems of the GI tract.
Frequently Asked Questions
ERCP may be useful in diagnosing and treating problems causing jaundice (a yellowing of the whites of the eyes) or pain in the abdomen.
ERCP can be helpful when there is a blockage of the bile ducts by gallstones, tumors, scarring or other conditions that cause obstruction or narrowing (stricture) of the ducts. Similarly, blockage of the pancreatic ducts from stones, tumors, or stricture can also be evaluated or treated by ERCP, which is useful in assessing causes of pancreatitis (inflammation of the pancreas).
Problems with the bile ducts or pancreas may first show up as jaundice or pain in the abdomen, although not always. Also, there may be changes in blood tests that show abnormalities of the liver or pancreas.
Other special exams that take pictures using X-rays or sound waves may provide important information for use along with that obtained from ERCP.
To understand how ERCP can help, it’s important to know more about the pancreas and the bile duct system.
Bile is a substance made by the liver that is important in the digestion and absorption of fats. Bile is carried from the liver by a system of tubes known as bile ducts. One of these, the cystic duct, connects the gallbladder to the main bile duct. The gallbladder stores the bile between meals and empties back into the bile duct when food is consumed. The common bile duct then empties into a part of the small intestine called the duodenum. The common bile duct enters the duodenum through a nipple-like structure called the papilla.
Joining the common bile duct to pass through the papilla is the main duct from the pancreas. This pathway allows digestive juices from the pancreas to mix with food in the intestine. Problems that affect the pancreas and bile duct system can, in many cases, be diagnosed and corrected with ERCP.
Depending on the individual and the types of procedures performed, ERCP does have a five to ten percent risk of complications. In rare cases, severe complications may require prolonged hospitalization.
Pancreatitis is the most common complication and may require hospital care, even surgery. Bleeding can occur when the papilla has to be opened to remove stones or put in stents. This bleeding usually stops on its own, but occasionally, transfusion may be required or the bleeding may be directly controlled with endoscopic therapy.
A puncture or perforation of the bowel wall or bile duct is a rare problem that can occur with therapeutic ERCP. Infection can also result, especially if the bile duct is blocked and bile cannot drain. Treatment for infection requires antibiotics and restoring drainage. Finally, reactions may occur to any of the medications used during ERCP, but fortunately these are usually minor.
Although most procedures are successful when performed by a trained physician, alterations in the anatomy or abnormalities found at the time of the procedure may not allow instruments to be placed inside the desired duct. This may necessitate an alternate procedure.